In our ongoing efforts to share more information about three-legged cats, we hope you enjoy this entire Tripawd Talk Radio podcast dedicated to Tripawd cats pain management tips and tricks!
Join us in a fascinating discussion about the feline pain medications, pill giving techniques and the latest developments for treating post-op amputation pain in cats.
Expert Stephen Cital Shares His Best Tripawd Cat Pain Management Tips for Pet Parents
Download this fascinating Tripawd Talk Radio podcast below (read the transcript below) for great tips about feline amputation recovery and beyond, such as:
- Why cats don’t always get good pain control
- How to tell your cat is in pain
- Why poor cat pain management can delay healing
- Tripawd cat pain control options to discuss with your vet
- The pain drugs for cats you want to avoid
- Best vet tech tricks to give medicine to cats
- Common cat pain management medication side effects in cats
- and more!
Our guest is Stephen Cital, RVT, SRA, RLAT, VTS- Lab Animal Medicine, a renowned veterinary nurse and educator from Northern California with a focus on veterinary anesthesia, exotic animal care and education for veterinary nurses. He has a long list of credentials as a Registered Veterinary Technician, a Surgical Research Anesthetist and a Registered Laboratory Animal Technician.
Stephen is also Executive Director for the Academy of Laboratory Animal Veterinary Technicians and Nurses and holds a VTS credential in Research Anesthesia. He also serves on advisory boards for local Vet Tech colleges, is on the Aratana Technician Council of Pain Experts, is an Advisory Board member for PhytoAnimal Health, and is COO for the Veterinary Anesthesia Nerds and Veterinary Cannabis Academy Facebook and webpages.
Tripawd Talk Radio#73: Tripawd Cat Pain Management Tips
Listen to this cat pain management episode here, or wherever you enjoy podcasts on Tripawd Talk Radio. Read on for the full transcript of our discussion about cat pain management with expert Stephen Cital.
While you listen:
- Find more helpful tri-kitty tips.
- Browse all Tripawds cat blogs.
- Download Cool Tips for Tripawd Cats
Read the Full Transcript: Tripawd Cat Pain Management Tips and Tricks
Intro: Thank you for tuning in to Tripawd Talk Radio where we’re spreading the word that it’s better to hop on three legs than limp on four, hosted by Jim and Rene and Wyatt Ray of the Tripawds Blogs Community at Tripawds.com. Serious talks for canine amputees and their people.
Jim: Hello and thank you for listening to Tripawd Talk Radio. Cat parents coping with amputation for their cats and anyone in veterinary practice will want to stay tune today. We are talking about managing feline amputation pain before, during, and after surgery.
At the 2018 Western Vet Conference, we had the pleasure of meeting our amazing guest who is an expert on this subject. Stephen Cital, RVT has all sorts of other initials after his name but in short, he is a renowned veterinary anesthetist, exotic animal specialist, educator speaker, and inventor of the Cital-Flow Practivet Blood Filter who was granted the 2017 California Registered Veterinary Technician of the Year Award. Well, he is incredibly knowledgeable and honestly, just really fun to talk to.
So, let’s discuss how to help manage amputation pain in cats. Thanks for joining us, Stephen. Welcome to Tripawd Talk.
Stephen Cital: Hello and thank you.
Rene: Hi, Stephen. It’s Rene here. I’m so glad we bumped you at the conference because you have an amazing background that I’m – that I need to hear more about. Can you tell us how you got into the veterinary field and why you chose this line of work?
Stephen Cital: Oh boy! Well, I kind of – I got into it on purpose and then kind of fell into it pretty heavy. When I was in high school still, I actually wanted to be a human nurse and I wanted to get exposure to medical procedures and being around medical things. And so in high school, I actually took a job at a general practice in my hometown in Woodland, California and started working as a kennel assistant and then they started training me as a veterinary assistant.
And then I started with human nursing school and then we started touching people and I was like, “Oh my God! This is not what I want to do.” People are kind of gross. But I really realized that I love the science and the medicine and I happen to really love animals. So I thought, “You know what? I should do the veterinary nursing track.” And that’s kind of how that happened. I didn’t intentionally go into veterinary medicine to be a specialist at anything but it kind of worked out that way. And I love it and I’m definitely not looking back.
Rene: Awesome. That is a great story about your people nursing experience. We can tell that you’re really great with animals. And I want to talk about cats today because we have so much information on Tripawds about dogs and that’s how we started as community. But we’re just now learning about cat’s needs before, during, and after amputation.
And in general, there’s just not a whole lot of information out there for pain management in cats. So let’s talk about that today. We see a lot of dogs come home from amputation surgery with a big bag of pain medications but cats, I mean they rarely come home with anything more than buprenorphine. I mean I don’t even know if I’m saying that right.
But why does it seem like in veterinary medicine that cats are getting the short stick when it comes to pain management? And do you think that’s changing at all?
Stephen Cital: I absolutely agree with you. I think cats have historically gotten the short end of the rope or stick of however you want to say that phrase. But I think the biggest misunderstanding or the biggest reason that cats aren’t getting the same level of pain management compared to our dog friends is because the practitioner maybe doesn’t understand the pharmacology of certain drugs with cats or cats are so good at hiding their pain and pretty stoic that they don’t necessarily look like they’re pain. But that’s not necessarily true. We know that cats and dogs are feeling the same level of pain because they’re both mammals and they both have the same nociceptor system.
That nociceptor system is that system that is responsible for transmitting pain signals throughout the body into the brain. So we know that cats and dogs have the same darn thing. We just don’t treat it the same because there’s a lack of education and lack of understanding on the practitioner side.
And this is really where I hope that we can have the nursing staff and the pet owners be a real advocate for their pet because it is something that needs to change. I would say in general it is changing but it’s changing very slowly.
Rene: And is that because there aren’t enough specific medications that cats do well on or they’re in the studies or does it just come back to like you said, a lack of understanding?
Stephen Cital: Yeah. The tricky thing with cats in general is they do metabolize certain medications differently than dogs. And we get a little bit more concerned about cats because they tend to not want to eat and drink as well after anesthesia, which can also be associated with pain. They don’t want to eat when they’re painful.
So it’s this tricky balance of getting them to do the right thing during the healing process and understanding the pharmacology of certain drugs. But in general, I would say we have a really good option for cats and there’s really at this point no excuse to not provide them with appropriate pain management.
Rene: Yeah. I love hearing that. Thank you. That’s a really great statement. Now, as far as cats showing their pain, you mentioned that they’re pretty good at hiding it.
Stephen Cital: Yeah.
Rene: But what are some of the things that they do tend to display? What are some of the behaviors? What can somebody look for if they think their cat might be in pain?
Stephen Cital: Sure. So one of the big things that we see with cats is we know cats in general do like to hide and like to have a lot of me time, right? But if they are increasing that frequency after a possibly painful like an amputation for sure, that is definitely an indication of discomfort.
If the animal is not eating or drinking normally, that is a sign of discomfort.
If they are not using the restroom with the same frequency, that is a sign of pain.
And this is going to be really shocking but purring can also be a sign of pain. Purring does not necessarily mean that they are happy all the time. We know that cats in the wild, they can purr at certain frequencies to actually heal the bone which is pretty amazing because we are trying to take some of that nature’s technology and apply it to humans in creating certain things that are creating the same frequency as a purr because it helps stimulate bone growth which is crazy, right?
Rene: Yeah.
Stephen Cital: So, even purring can be a sign of discomfort. What else is a sign of discomfort? Definitely a change in personality. If the cats are not wanting you to scratch them in the normal areas or be it social, those are all signs of discomfort.
And then one thing I think owners can do is I’ll actually post it on my website because it will make it easier to find but the International Veterinary Academy of Pain Management has a really nice chart for owners on signs of pain in cats. And that’s nice to have on hand so you can be like, “Oh, my cat has this, this, and this. I think he might be uncomfortable. Let’s talk to the pet about more pain meds or pain meds in general.”
And then the other thing which is nice and owners can use and a lot of hospitals are using now are called visual analog scales. And they’re validated by scientific studies. And they are akin to the smiley face chart that you see when you go to the doctors and the doctor says, “Hey, what smiley face are you? Is this minimal to no pain or is it severe pain?” So it’s kind of like that smiley face chart for cats specifically.
And then more recently, we even have a published paper now and it’s coming out of the Lab Animal World and it’s actual pictures of cat’s faces. It’s another visual analog scale of cat’s faces when they’re uncomfortable. It shows their position, their eye position, how squinty their eyes look, what their pupils look like. So it looks at all of that. And I think that’s just a really great tool for owners to have because you can see, you can actually see what a painful cat would look like.
Rene: Oh my gosh! When is that tool coming out? We would love to have access with that.
Stephen Cital: Oh, it’s out already. It’s out already. And I will gladly put it on my website for anyone to download. But it is out, yeah.
Rene: And what is your website, Stephen? We’ll say it a few times but go ahead.
Stephen Cital: Yeah. My website is www.StephenCital.com and I’ll put in my resources section so owners can download it. And they actually have the same thing for dogs with the exception of the photographs of the faces. That’s where cats actually have the leg up compared to dogs.
Rene: Oh, OK. Yeah. Actually, the photos were the ones that I was thinking of, the IVAPM one. We actually do have a link to that but put it on your website too so people have access to it.
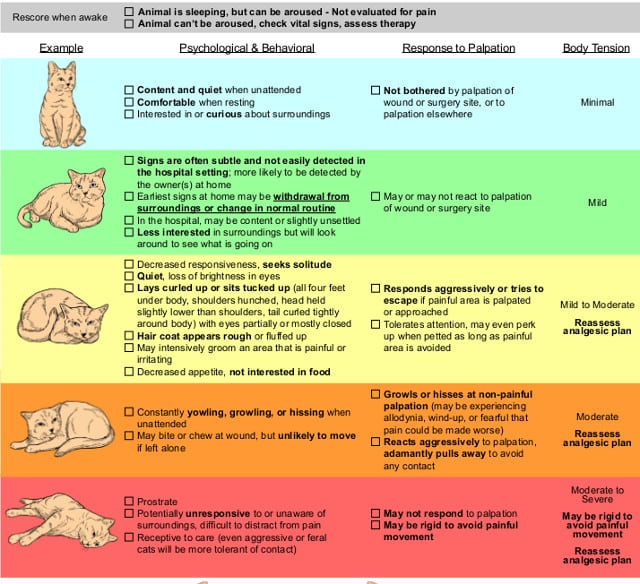
IVAPM Cat Pain Management Scale Chart (download here)
Stephen Cital: Yeah, absolutely.
Rene: But yeah, the photos would be really interesting to see because I personally know that I had no idea of what pain in dogs look like until we looked back on our own dog after he recovered from amputation surgery and we saw the before pictures of him and we were just blown away. We put them side by side and went, “Oh my God! Look at his ears. Look at how he is standing. This is crazy! How could we not see this?”
Stephen Cital: Yeah. And I mean dogs are a little bit different than cats too because they still want to appease you even after a surgery where cats are kind of like, “I’m not as interested in appeasing you after I have my leg amputated.” So yeah, there are definitely differences.
Rene: Definitely. Now, just real briefly now, you have worked with some pretty big cats in your past, right? That’s something I didn’t mention in the beginning. Can you tell us more about that?
Stephen Cital: Well, I do per diem a couple of zoos and have certainly worked with cats and tigers or I’m sorry, tigers and lions. They’re all cats. And what’s interesting about cats in general whether they’re a big exotic species or domesticated species like the one at home is they’re pretty genetically conserved.
So even these cats that we have at home that get renal disease or get these common conditions that we see in pet cats, our big wild animal cats get those same things, and we have to treat them the same way and we give them the same medication. Yeah, it’s really interesting. They’re so well-genetically conserved that they suffer from the same conditions.
Rene: Holy cow! And I thought we could blame all of the domestic illnesses on [0:11:28] [Indiscernible]. So it’s not that scary.
Stephen Cital: No.
Rene: And do wild animals, do they show pain similarly to domestic cats?
Stephen Cital: Absolutely. So like I mentioned with dogs, they still have that appeasement behavior. They still kind of have that pack mentality. I don’t want to get too crazy because I don’t want to say that the whole alpha dog thing. I’m not a firm believer in that type of behavior for dogs.
But for cats in particular, domestication has changed a little bit of their behavior but in general, it is still the same as like our lions and our tigers and our cougars and whatnot.
Rene: Wow! Well, you certainly know all about cats. We’re so happy to have you here. Now, let’s talk about managing surgery pain for our domestic cats. How does the pre and post-amputation pan management protocols, how do they differ for cats as opposed to dogs both in the clinic and then later on when you get them home? What are the differences there?
Stephen Cital: Sure. So in reality, there shouldn’t be any differences.
Rene: OK.
Stephen Cital: There really should be any differences. I would say the major difference that we see in cats compared to dogs is the veterinarian being more hesitant to use a nonsteroidal anti-inflammatory. And the reason they get more wary about using a nonsteroidal ant-inflammatory is because cats when they go under anesthesia, they can get a little hypotensive at time. So that means their blood pressure get slow.
And if our blood pressure gets low, we’re impacting our kidneys. So we don’t want to put extra stress on our kidneys. And when we give a nonsteroidal anti-inflammatory, those nonsteroidal anti-inflammatories create these little things called prostaglandins. And the prostaglandins keep your kidneys and your GI healthy.
And so, if we knock those out and we have a hypotensive event, we’re putting our cat at more risk or potential for risk of side effects when they wake up. So I think that’s the big scare. But if you have a really good anesthetist and a practitioner that’s using a balanced anesthesia protocol, that shouldn’t be as big of a concern because we can maintain that blood pressure better.
But one thing that we can certainly do and all cat owners should really advocate for is the use of nonsteroidal anti-inflammatories in their cats in the pre-operative or immediately post-operative period because inflammation is pain and obviously, when you’re taking off a limb from anything, there is going to be a lot of inflammation there and if we can cut that inflammation before it really happens, it’s going to be in our pet’s best interest, if that makes sense.
Rene: Yeah, that totally makes sense. And so, what are some of the brand names that we as cat parents might be familiar with as far as the NSAIDs?
Stephen Cital: Sure. So for the nonsteroidal anti-inflammatories, a common one that we see in practice is we see meloxicam. There is a drug that I kind of prefer in our cats because it works a little bit more locally than systemically, which adds to its safety profile and it’s called Onsior. And the generic name for that is called robenacoxib. And that is a drug that is going to work at the local side of inflammation rather than systemically. So we have less concern about renal or liver or GI concerns.
And the box dose right now actually has it labeled for three days. But off label and validated by some scientific studies that I believe was published in the journal of internal medicine, veterinary internal medicine, they have studies going out 28 days with this particular drug and showing no detrimental effects. So that is one I definitely like to lean on.
And whenever we have a cat that is going to be on NSAIDs, it’s really important that they’re eating and drinking normally. Hydration is going to be super important to keep those kidneys running normally especially when we’re giving something like an NSAID.
Rene: Are there any special considerations for senior cats or diabetic cats when it comes to the NSAIDs?
Stephen Cital: For older or diabetic cats, again, it’s just going to be that hydration. Keeping them well-hydrated while they’re on the drugs and then definitely give them the benefit of an NSAID. When we have animals that are stressed out or painful, pain is a form of stress and you release more cortisol, it can definitely affect the diabetes process or disease. It can make it worse. It can exacerbate it temporarily. So that’s not something we necessarily want.
And the release of cortisol in itself is also going to delay wound healing. And it can even suppress the immune system. So it’s in our patient’s best interest to provide really good pain management and multimodal. And when I say multimodal, that means multiple different drugs, not just one drug like you mentioned at a high dose.
And what’s nice about mixing different drugs or doing polypharmacy is when you mix different drugs, some of these drugs play really nice together and they can potentiate each other so it makes them work better and we can use them at lower dosages, which is going to get rid of some of the negative side effects we would see with a big, huge dose of buprenorphine or a big, huge dose of a particular nonsteroidal anti-inflammatory.
Rene: Oh wow! That is really interesting. So what are some of the combinations that you tend to see in practice?
Stephen Cital: Yeah. So one of the big things is when you use an NSAID appropriately, you can decrease and opioid dose by almost 40%. That’s a huge, huge decrease in how much opioid we’re giving that cat. And as you know just like in people with chronic opioid use or high doses of opioids, it can slow your GI tract and it can create some constipation which isn’t necessarily fun when you maybe have back leg that was just removed and you’re trying to learn how to squat again, right?
We can get them to eat a little bit better because when they’re on NSAIDs or not NSAIDs, opioids, they may feel a little bit nauseous from those opioids in particular.
Other things that we see work really well together are things called benzodiazepine. So those are things like valium or midazolam. And when you mix those with an opioid, we can significantly decrease the opioid dose as well.
Rene: And is that because it mellows the cat out because that’s what I think of when I think of a drug like that.
Stephen Cital: It certainly mellows them out. But it also – it works as a – if you think of an opioid molecule and it’s in the body and then you think about adding a benzodiazepine, the benzodiazepine molecule acts almost like shepherd for that opioid molecule and helps it get to that particular receptor it’s supposed to work at better.
Rene: Cool! Wow! I am learning so much from you. Oh my gosh! So now, how can we know that our vet is practicing really good pain management like this? Because normally, we go on as cat parents and our pets are fine and we take them for their checkups and then wham! We get hit with news that their leg has to come off or they need some other type of major surgery.
And all of a sudden, we are forced to figure out this whole pain thing. We don’t know anything about the drugs. We don’t know what our vet was really using during surgery. I mean how do we know that our clinic is going to use the best and safest pain management methods?
Stephen Cital: Sure. So as kind of a pain management enthusiast, there are a couple of things that I like to really tell owners and personal friends when they ask me, “Oh hey, can I go have surgery on my pet? What should I look for or be concerned about?”
And the biggest thing we have to be concerned about right now especially in cats and especially since we’re in an opioid crisis and a lot of clinics are struggling to get appropriate opioids for this big type of procedure is to stay away from a drug called butorphanol.
Yeah. Butorphanol is a common drug that we use in veterinary medicine. It is a pain medication but it’s probably only lasting for like 30 minutes to maybe 2 hours once we give it. And the animal can still looks sedate even after that 2-hour period but it doesn’t necessarily mean they’re getting the benefit of pain management.
And unfortunately, a lot of more mature veterinarians or older or grey-haired veterinarians still uses pretty commonly and it’s really not a good pain management drug. So if your animal is going to have surgery, make sure they get a really good opioid, something like methadone or hydromorphone or fentanyl even if they can get their hands on it during the procedure and after the procedure, not butorphanol.
Rene: Oh, that is really good.
Stephen Cital: Yeah. The other thing that I would really advocate for any pet owner to ask about is using local anesthetics at the site, so using things like lidocaine or bupivacaine after and before they are taking that leg off. Lidocaine or bupivacaine is the only pain management drug that we have on the shelf that completely blocks the pain signal. When we give things like opioids or NSAIDs or gabapentin, it’s only dulling the pain.
But things like lidocaine and bupivacaine are the ones that completely stop that sensation all together. So that’s pretty profound. And if they use them correctly, we can really minimize how much systemic drugs or oral drugs we have to give the animal when it wakes up.
There is a company called Aratana and they create a bupivacaine that is encapsulated in liposome and that block lasts for 3 days once you inject it. So that cat can feel pain-free for 3 days. It is off label at this point. Right now, it’s only labeled for dogs for CCL repair. But there is going to be a cat label released hopefully this year but I would say at a personal experience and talking with other anesthesiologists and anesthetists, we’re using an off label for cats all the time and we’re seeing great success with it.
Rene: That is pretty cool. And I’m going to guess but I think you’re referring to the one that I know as NOCITA. Is that it?
Stephen Cital: NOCITA is it, yeah.
Rene: Awesome. Yeah. When we first heard about that, we were so excited. Dr. Mike Petty told us about it.
Stephen Cital: Yeah.
Rene: We have a little blog post about it for dogs. But I can’t wait until we can start announcing it because it’s being used for cats.
Stephen Cital: Yeah. It is a game-changer.
Rene: Definitely. And one thing that I get really excited about is because it means that you’re not shoving a whole bunch of pills down your pet’s mouth as soon as they come home from the hospital when they’re already pretty dopey and stressed out. So let’s talk about that.
What are some of your best tricks if we have to give those pills to a cat, what are some of the things you as a nurse get to do that actually work?
Stephen Cital: Right. So the biggest thing is if we can get liquid, that is always easier. And a lot of pharmacies will compound different pain medications so that we can give it in a liquid form because pills can certainly be tricky for cat owners.
And the other trick as a technician that I do a lot is I do manual pilling and it’s really sticking that pill on the back of that cat’s throat and pushing it down there with a finger. And it’s really quick. But cats unlike dogs are really good at swallowing things the first time compared to our dog friends that can hide things in the back of their mouth and somehow get it up. I’m not really sure how they do it.
But our cat friends when it’s done appropriately, they usually take it down on the first swallow so that’s really nice. And that’s where asking for a skilled technician to come in and show you how to pill your cat is going to be really, really beneficial.
Rene: Oh, yes. So many people are terrified of that. So thanks for that tip.
Stephen Cital: Yeah. The other thing that pet owners can do when appropriate is ask for drugs that are long-acting and injectable. So there is a drug on the market called Simbadol and it’s a buprenorphine and instead of giving it under the tongue or in the cheek like we would normally, it’s one injection and it lasts for 24 hours.
Rene: Oh, wow!
Stephen Cital: Yeah. So it kind of alleviate having to give three doses of the buprenorphine a day with this one injection.
Rene: Yeah. Yeah. That is really cool. These drugs are getting better all the time. Real quick, just to backtrack, you had mentioned about the opioid shortage that’s happening, is that in full-swing right now?
Stephen Cital: It is. It is in full swing. It is pretty horrible. I speak all around the country and I just listen to these – some of them have nothing and I’m just like it’s just so, so, so horrible. But yeah, it’s pretty dramatic. But I think the nice thing that’s coming from it is it’s forcing veterinarians to reevaluate their pain management protocols and really update it.
One thing in particular for amputations, because we’re cutting some major nerves, is it can set your animal up for what’s called neuropathic pain. And neuropathic pain is also discussed or described as something like a phantom limb pain or the animal keeps chewing up their amputation site because that nerve is still sending signals.
And there are certain drugs that we have in practice that can really help decrease that type of pain. And one of them is ketamine. Ketamine is a great analgesic and it’s great for anesthesia because when we add ketamine to an anesthetic protocol, we can decrease how much gas anesthesia we’re giving which is going to increase our blood pressure, keep our blood pressure as normal as possible. But it’s also going to keep the special receptors, the NMDA receptor cool, calm, and collected so that we hopefully don’t get into those wind up states or neuropathic states.
Rene: Ketamine. You’re just referring to cats, right?
Stephen Cital: Cats and dogs.
Rene: Really?
Stephen Cital: Absolutely. Absolutely.
Rene: Oh, cool! That is really good to know. That’s what I haven’t heard mentioned a lot. But I’m glad you mentioned neuropathic pain because we see that a lot and probably more than anywhere else on the internet because there are all these cats and dogs and their few limbs and people don’t know how to treat it.
Gabapentin tends to be the go-to prescription when somebody goes to their vet. Is that always successful in cats?
Stephen Cital: So what’s interesting is there was this – we’re still in the middle of this kind of like paradigm shift of not using tramadol as much. And so, when we have the studies come out suggesting that tramadol does not work well in dogs for pain, everyone kind of switched and jumped on the gabapentin train.
And what we found in dogs is gabapentin actually isn’t working that awesome for pain. It’s definitely helping but it’s not working as good as we thought it was. But in cats, we have actually found that it does work moderately well. So that’s good. I’m so happy and I’m less disappointed because it is actually working well in cats.
I forgot where I was going with that. But …
Rene: No, that’s OK. I mean so when somebody’s vet prescribed it for phantom pain, they should feel pretty good.
Stephen Cital: Absolutely. Absolutely.
Rene: Most likely going to work. Awesome.
Stephen Cital: Yeah.
Rene: So I’m a really bad host here. We’re already at the 30-minute mark. I want to ask you real quickly though if you have time, what are some of the common side effects that we should be on the lookout for when our cat comes home and they’re given these drugs? What are some things that are telling us this is too much or too little medication for them?
Stephen Cital: Yeah. The biggest thing that I would say is a point of concern is vomiting and possibly stool changes, so maybe some diarrhea. Those would be suggestive of the medication really not sitting well with their body. And it can potentially put your pet in danger of becoming super dehydrated. And again like, dehydration is kind of our worst enemy when we’re using NSAIDs and other medications all together. So I think those would be kind of my top 2 things.
I would definitely expect to see a little bit of lethargy or them being kind of quiet because of some of the medications that we’re sending home. But after an amputation, like that’s maybe not the worst thing in the world, giving of a couple of weeks to just kind of chill out and heal is OK.
Rene: That is really, really good to know. And Stephen, I can’t thank you enough. I could talk to you all day about this. You are so knowledgeable. We’re so grateful to have you here. Thank you so much.
Stephen Cital: You’re welcome.
Jim: Yes, Stephen, thank you so much. That was fascinating. Listeners can learn more cat pain management and all the other work you’re doing with all sorts of animals at StephenCital.com. That’s S-T-E-P-H-E-N-C-I-T-A-L.com. And find many more helpful pet pain management articles, podcasts, and video interviews at Tripawds.com.
Outro: Until next time on Tripawds Talk Radio. Learn more about canine amputation recovery and find the best gear for 3-legged dogs and cats at Tripawds.com.
[End of Tripawd Cat Pain Management podcast transcript]
Find other Tripawds News posts about cat pain management.





Excellent interview!! A must listen or read for ALL cat owners!
Yes, NO more short sticks for cats. I love Stephen addressed that cats and dogs are both mammals and feeling the same pain! YES, THE SAME and cats hide it more! Same and we don’t treat it the same! Subject drives me bonkers.
Multi/drugs!!
Good options for cats and NO EXCUSE for lack of pain management for cats! We MUST advocate for our cats.
THANK YOU! <3
Yay Holly I’m so hoppy you liked the interview. You inspire us to continue reaching out for more feline Tripawd information. They absolutely deserve to be treated the same!