Many pet parents and even veterinarians don’t know about the benefits of rehab therapy for Tripawds. That’s why today we hope you’ll tune in to Tripawd Talk Radio Episode #117. We chat with Dr. Ana Esquivel, founder of Ace of Paws canine rehabilitation therapy in Albuquerque New Mexico.

- Discover the benefits of canine rehab for Tripawds, especially during recovery from amputation surgery.
- Learn about the best therapy treatments for three legged pets
- And we also discuss how to find a good therapist for your Tripawd hero.
Join us as Dr. Ana Esquivel explains all that and more on this episode of Tripawd Talk Radio. Listen, watch, and read the show transcript below!
Listen to Tripawd Talk Radio Episode #117: Canine Rehab for Tripawds
Watch on YouTube: Tripawd Talk Radio Episode #117: Canine Rehab for Tripawds
About Ace of Paws & Dr. Esquivel
Dr. Ana Esquivel is a practicing veterinarian in Albuquerque, New Mexico. Long ago she recognized her geriatric patients were in need of special attention. They needed more than the typical drug therapy prescribed for their pain management.
Because of this, Dr. Esquivel became more familiar with aging canines’ physical needs. SHe learned how to maintain mobility and a higher quality of life. Studying Medical Acupuncture for Veterinarians revealed that most of her patients could benefit from more than the prescribed drug therapy for their pain management.
In 2018, she became a Certified Canine Rehabilitation Therapist. Today she is founder of ACE of Paws, the only dedicated Canine Rehab Clinic in Albuquerque New Mexico.
Remember, Your Tripawd Can Get Free Rehab Therapy

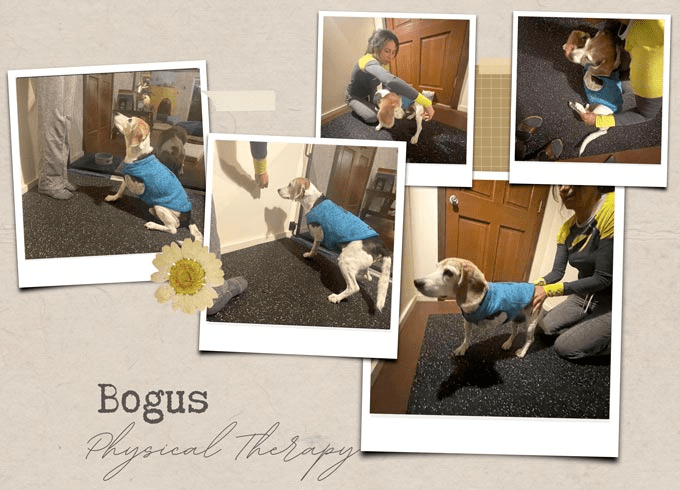
Three of Dr. Esquivel’s patients are recipients of our Tripawds Rehab grant! This fund reimburses anyone who take their three-legged dog or cat for rehab evaluation by a certified therapist. We hope you will do the same!
Important Tripawd Talk Show Links
Ace Of Paws:
https://www.aceofpaws.com/
RESOURCES
How to find Canine Rehab for Tripawds:
https://tri.pet/findrehab
Tripawds Rehab Reimbursement Grants:
https://tripawds.org/rehab
At Home Rehab Programs:
https://tri.pet/athomerehab
Tripawd Talk Radio Podcast Transcript
The Benefits of Canine Rehab for Tripawds
TRIPAWDS: Thank you for joining us, Doctor. And welcome to Tripawd Talk.
Dr. Ana Esquivel: I’m glad to be here.
TRIPAWDS: Dr. Esquivel, can you tell me how you got into rehab therapy?
Dr. Ana Esquivel: Absolutely. So my journey with rehab started back in 2017. So my own dog had lots of orthopedic issues and after she had her third knee surgery. I was just having a lot of trouble getting her back to just being active and was still having lameness issues. She just wasn’t recovering as well as she had prior to surgeries.
I reached out to a fellow veterinarian who is doing a little bit of rehab inside of the ER. She is kind of doing it more part-time. And she had an underwater treadmill and I was like, “My dog needs an underwater treadmill. She needs this to help her get back in shape.”
And after talking to her, she is actually a Certified Rehab Therapist, but has taken time off and come back. She is still around but not seeing patients as a regular clinician. And so, I was talking to her and I was just like, “How do I get into this? This seems really interesting to me. Obviously, my dog needs this and how do I get my dog a treadmill? How do I learn how to do this right?”
She did the University of Tennessee program and I started looking around and I found Canine Rehab Institute. They were a lot closer and a lot more of a hands-on type program and so I really like their program and it was in Colorado, which is where I had gone to school and some of the professors were affiliated with CSU as well.
So I was just like, “I’m going to check this out.” And I started the certification in 2017.

It took about a year or so because it’s – we go for a couple of days at a time and they offer classes throughout the year. And so once you finally get it all done, it takes almost a year to complete.
And at that point, I was still in general practice and I still see tons of geriatric patients. I got all these dogs and throwing all these drugs at them and nothing is working. And I was like, “I need to have another tool in my belt.”
When I was in vet school, I actually – in my senior year, I actually learned acupuncture. And back then, this is almost 15 years ago, acupuncture was still new to veterinary medicine. I was already interested in alternative and complementary type medicine. I didn’t really use my acupuncture very much in general practice.
Then I was just like, “I really need to just do this more. I need to give people more than just hey, here are some more drugs.” So that’s kind of how it really came about is like I wanted to do more of the alternative and complementary medicine. Just because when you’re throwing all these drugs at them and nothing is working, what do you do next?
I ran into that with my own dog. It’s like when she developed kidney disease and then eventually she developed cancer, it’s like there’s only so many things you can do and you have to find other ways to help them. And some of it is palliative and some of it is just simply strengthening and just that mobility like I got to keep my dog moving.
So that’s kind of a roundabout way of how that actually came about.
TRIPAWDS: That’s awesome. At what point did you found ACE of Paws? That’s in Albuquerque, correct?
Dr. Esquivel: It is. So ACE of Paws started officially in September of 2019 so we have officially made it to three years.
And all the way through COVID and COVID nearly wiped us out. We had to basically – we don’t even open maybe 6 months, maybe right before COVID started. And so, we pretty much lost all of our clientele because of COVID, shut down and everything.
Because we were working with geriatrics, a good portion of them passed during that time. And we took a good 6 weeks off during that time. I was still working as a general practitioner so I was still working full time and transitioning into my own business.
I was doing both of them part-time and slowly we’ve gotten to a point now where we are open a full schedule or open 4 days a week and we are seeing patients all the time and it has grown immensely over – and a lot of it is just are referring veterinarians, are word of mouth, just slowly building the practice.
TRIPAWDS: What suite of services does ACE of Paws offer?
Dr. Esquivel: I try to offer a very wide variety of things because there are some things out there that people are starting to or I should say veterinarians are starting to offer that are in the complementary realm.
There’s certainly more acupuncture now than there was in the past. I’ve got colleagues that have gone and done the same training that I did and they offer that. A lot of places are starting to offer laser therapy as well, which laser is one of the things that I used on pretty much every dog I see.
Acupuncture I use quite a bit for the neuro and definitely orthopedic type cases but I definitely like it for my neuro dogs, my back dogs. We are trying to get these paralyzed dogs back up and walking. And so, those are kind of the ones that you could find. It’s not necessarily rehab-specific. B
Because I am a rehab-only clinic, we offer things like PEMF which is pulsed electromagnetic field so that in the form of like an Assisi LOOP or a bed while they are getting treatment.
The laser therapy, sometimes we do manual therapy, depending. And my technicians are trained in massage so some of that is joint manipulation which is me, whereas massage is more them.
The underwater treadmill is a great tool for a lot of dogs. You don’t always need it. There is definitely a lot of practices out there that don’t have a treadmill.
You can certainly do rehab without it but it’s a really awesome tool to have especially when you are trying to teach them how to walk again or just simply fitness, fat camp. You are trying to get these guys to lose weight, and they can’t walk and they are so sore and it’s a variety of things.
Let’s see what else. A therapeutic ultrasound, we use that a lot for dogs who have shoulder issues, tendinopathies. We just got a shockwave machine so shockwave is really good for pain. We have been using that a lot for our cruciate disease, hip dysplasia, all these dogs. And those are especially important with our tripawds because they like to development arthritis and a lot of them are – if they’ve got cancer or if they’ve got some other concurrent disease, they’re going to develop arthritis so much faster.
I just got the shockwave – actually, it has been a couple of months now. I think we are only 6 months and I’ve been using it quite a bit as a new tool to the practice. But we have a wide variety of things.
TRIPAWDS: Why is rehab therapy beneficial for tripawds in your opinion? What can it do for them?
Dr. Esquivel: So kind of depends on like you said, where you find them.
- If they are a brand new tripawd and if you are lucky enough to have a clinic that it’s kind of a surgery center and they might have a little rehab department, and a rehab department might only be a room that has a treadmill in it and a little exercise floor or whatever. They still can do some stuff.
- In that immediate post-op period, they can implement therapy right away, and that can be in a form of icing or doing cold compression right immediately after surgery.
- If they do have a laser, they can laser that incision site. They can do things like tense therapy for muscle relaxation.
TRIPAWDS: That’s that little machine with the sticky pads?
Dr. Esquivel: Yeah, the electrodes. If you go to a chiropractor a lot of time, they put those on you and yeah, it helps relax your muscles and it feels a little tingly and it feels really good. You can do that with dogs. And you have to shave them a little bit but yeah, you can do that with them.
You can start range of motion. So they can get them started right away essentially. So if you got a practice that offers those types of therapies, obviously, it’s kind of that general nursing care. You can essentially start day one.
Where I typically see them because I am a rehab-only practice, I don’t usually see them until about 2 to 3 weeks later after they’ve already had their recheck with their surgeon. They’ve had their suture removed and all of that and the surgeon said, “OK, everything looks good. You guys can go on your way.” They usually give them some generic like, “Oh, yeah, just start walking a little bit. Get him up into and maybe do some range of motion.” They don’t really know what to tell them to do.
I get in there and give them like, “This is what we are doing. This is the program we are going to follow. This is how we are going to get your dog working better.”
Dr. Esquivel
TRIPAWDS: There are still so many vets out there that say, “They will be fine. Just go let them be a dog.” So why do you think that is? Are these vets not…?
Dr. Esquivel: Yup. Well, I never learned it. I mean I’ve been in this field almost 20 years and I didn’t hear about rehab or really like know about it until 6 years ago.
Now, you’ve got schools that are actually doing it as a rotation. They are teaching it in their program. So Colorado State has it. Obviously, some of these other schools are finally starting to develop a natural rehab program and they are working with certified therapists that are running their program for them.
And the therapists aren’t always veterinarians. Sometimes they are human PTs that have gone and gotten certified. And so, that’s also in the realm of we are getting the word that more people are learning that this exists.
I have that problem in my practice is I have so many clients that come and say, “I had no idea rehab was a thing.” And certainly, the veterinarians, they might have heard about it but they don’t understand the value of it for their patients.
When we first opened, we had to go around to every single clinic in town and be like, “Hey, we are in town. We have these services. Send us your clients. We can help them.”
You don’t have to say, “Oh, my dog is 10 years old and here are some drugs and I don’t know what else to do for you.”
Dr. Esquivel
TRIPAWDS: When it comes to tripawds, how soon do you like to see them? What’s the ideal timeframe that somebody should go see a therapist?
Dr. Esquivel: I try and see them right away. I mean as soon as possible. So if they’re a new client like I said, right after surgery, we try to get them in in that 2 or 3-week post-op period if we can.
If they are contacting us and they are saying, “Hey, my dog just had surgery. I want to know what I can do.” We try to get them in after that 2-week recheck with their surgeon and they’ve gotten the OK.
If they are a client already and it might be they just got diagnosed with cancer or what have you or they broke their leg and it’s something irreparable that we already have that established relationship with them, we may do some pre-rehab. Then we will them even the week after surgery and just do some of that nursing care, trying to get them up, trying to get that flowing down, trying to do things to help heal that wound as fast as possible and get them up and moving.
TRIPAWDS: So wound healing is a part of therapy too, right? Even that incision needs some kind of extra TLC?
Dr. Esquivel: Yeah, absolutely. And we don’t want to develop a lot of swelling area. We want to increase the circulation to the area. Even just simple massage and things like that and icing can definitely bring that swelling down. We want to watch for infection or dehiscence of that incision site. That just puts us behind and it’s extra stress on the body and things like that.
It’s nice to have professionals who are – when the owner doesn’t recognize that there’s a problem, we are like, “Hey, there’s a little drainage or there’s a little spot here or this is really hot,” like there’s something going on underneath the surface. It’s nice to have even just a technician who can recognize, “This doesn’t look right or maybe it’s a little stinky.”
TRIPAWDS: We hear it all the time when people say, “Oh, he is not in any pain. He sits down on his walk or he keeps scooting along but he is not in any pain.”
Dr. Esquivel: I hear it all the time. “Oh, he’s limping but he is not painful.” I don’t understand the disconnect here. If you sprained your ankle, you’re limping. You’re hurt. You’re in pain. And yeah, I fight with a lot of clients on that.
Your dog is not going to scream. Your dog is not going to cry, unless maybe he is a little Chihuahua or some little – one of the little toy breeds. They are a little more dramatic. But your German Shepherd, your Golden Retriever, your Labrador, they’re just going to lay there and act like they’re fine because they’re so stoic. They are going to play through the pain.
Dr. Esquivel
I deal with a lot of geriatrics that the slowing down that people will say, “Oh, he is just getting old. He is slowing down.” That’s under diagnosed arthritis that they don’t recognize that as pain, as mobility. We lose so many of those older big dogs that should be mobile when they’re 10, 12, 14 because they didn’t recognize it early enough.
Dr. Esquivel: I get a lot of people who are like, “Well, I don’t want to give him pain medication for the rest of his life. I’m so scared of pain medication.”
And definitely in the human world, we have a problem with opioids. There is a lot of – I think there’s a lot of stigma around that that pain medication is bad and we have to kind of rework it in our brain that not all pain medication is bad.
And I know I have chronic pain issues and I had an orthopedic guy tell me, “You need to go do yoga. You need to go get acupuncture. And You need to go do these things. You need to get healthier so that you don’t have to take pain medication.” And I flat out told them like, “I don’t want to take opioids. I don’t want your drugs. I just want to know how to fix myself.” And I was very happy that he wasn’t a pill pusher and said, “Here, take these drugs.” He actually was like, “Hey, go do something better with your body.”
I feel like I get a lot of people wait too long. They just – and there is an appropriate time for pain medication. Absolutely – if your dog is painful, it’s limping, you need to get that inflammation under control.
You need to get that pain under control because your dog isn’t going to move and you get stuck in this vicious pain cycle where they’re not moving, they get more stiff, they get more painful, and it just keeps going back around and around and around and you get stuck in this chronic pain loop.
Dr. Esquivel
And pain medication has a place but we can also combine that with laser and acupuncture and some of these other things and strengthen those muscles because there’s weakness there or there’s a trigger point there or there’s just something there that’s preventing us from correcting that pain. So you got to get these guys moving. You got to get them up and moving.
Pain medication is great, but I want to use the smallest dose possible that keeps them going. You’ve got to get them to a maintenance where they might have a bad day and they might need pain pill but for the most part, they are comfortable all the time. That’s the goal.
Dr. Esquivel
TRIPAWDS: When you meet with somebody and they talk to you for the first time, what can they expect? Are they going to have to keep the dog on pain medication or will there be a time when they can decrease it because they’re adding in other things?
Dr. Esquivel: Typically, they are going to still be on pain medication like I said in most cases, if they’re immediately post-op. Some of them when I see them, if it’s a month or two later, they might not be on meds.
Part of my evaluation, what I’m looking for is, are they – do they have pain somewhere in their stifle? Do they have pain in their hip? Do they have pain in their elbow?
alot of times especially starting out, if they have never really done anything more than just walking, we will often put them back on pain medication or tell them, “Hey, give him a pain pill right after a session because they’re going to be sore.”
It’s just like us. You haven’t been to the gym in two years because of COVID and you go do 50 pushups and the next day, you’re going to feel that and you’re going to hurt and you’re going to say, “Why on earth did I do that?” And so, I’ll often tell them, “Give him a dose that night. It will help them be more comfortable.”
If it’s a more active problem that I find on my exam, I’m going to say, “Oh, let’s do a week or two and see how they do.” And if they are doing better, then we slowly wean it off.
the goal is to get it like I said, to the lowest possible dose and still keeps the dog moving, still keeps the dog comfortable.
Young dogs are going to recover a whole lot faster and they are going to be fine without pain medication. But my older dogs, they’ve got other stuff going on. They got arthritis in these other joints that unless you actually go and x-ray that dog, you may not find it and they are just showing us kind of that subtle, “I don’t really want to move my knee that much or I don’t want to – my range of motion…”
An owner is not going to recognize that. And that’s where the therapist is a good helper in that we are going to look at the full dog. We are going to look at their muscles. Then we are going to look at their range of motion. We are going to look how they are walking because I can’t tell you how many times they’re sent to me for one problem and I find three more.

TRIPAWDS: what would be the one reason for someone to see the specialist versus their vet?
Dr. Esquivel: Yup. So when I was in school, basically it’s, “Lameness, always hurting, two weeks of pain meds and put him on crate rest. Everybody started that. Try it for two weeks, see if it works. If not, come back.”
Sometimes they are doing x-rays that day. Or sometimes they are not. Sometimes they wait 2 or 3 weeks. In the meantime, that dog is just getting weaker and weaker and weaker. And that’s what I – the difference in coming from general practice and coming into this is I’ve learned that that’s so detrimental to these dogs that you can always just throw them in a creek.
And that there are even studies I think mentioned back from when I took this class that 2 or 3 weeks in a crate, you start to lose muscle. It doesn’t take a lot of time with rest to lose muscle. And we got to be very careful. Obviously like case by case is different.
A different recommendation we had if you are a neurologic patient. Neurologic patients are very different because they have to have that crate rest, that strict create rest because we don’t want those dogs to become more paralyzed than they already are if they are on the edge and that disc is about to blow. We don’t want them running around the yard.
And so recommendations will be different for a neurologic patient. They might be in crate rest for four, six weeks and it’s literally you go potty, you come back inside on your crate. Very different than a dog who just has an orthopedic issue.
It’s more about like OK, well, we got to put them on a leash and maybe only go walk for 5 minutes and you go for your potty break and whatever. But we don’t want them to do exhibits around the yard and we don’t want them going up and down stairs and parkouring off of furniture.
But yes, they do need some restriction but that whole crate rest and 2 weeks of Rimadyl doesn’t work for everybody. I found that it’s very detrimental to some of my patients. Certainly, if they have a fracture or something like that, there are different scenarios, but we are just talking like in general.
TRIPAWDS: Once you’ve evaluated some of these dogs, what does the program look like as far as length of time and how much of a commitment there is? I think a lot of people are scared that they have this thought, “Well, is it going to be like a chiropractor?” All these expensive visits.
Dr. Esquivel: Basically, I do my exam and there are a couple of things that happen during the exam.
I’m looking at their gait.
I’m doing measurements of their muscles.
I have one of those fancy little stance analyzers that actually tells me how much weight they are putting on each foot.
Sometimes it’s more subtle lameness and I’m like, “I don’t know what leg this is,” and I’m having to sit there with my slowmo and my video trying to figure out like are you limping on that leg? Are you limping on this leg? The analyzers helped a lot. I actually just got it here recently and definitely in the more subtle ones where I’m like, “I don’t know. Is it really that leg?”
It just kind of helps me with one more tool to see it. And sometimes it’s just like you start doing range of motion on a joint and you’re like, “Oh, there’s a pop. There’s a click there. Oh, you don’t bend this leg as well as you bend that leg.” So I look at the whole dog.
And oftentimes like I said, I’ll find it’s like, “Oh, he just had an FHO and he is not really extending that hip but then there’s something going on in the front leg, that’s the opposite front leg because now he is putting all the weight up there so now his wrist is ouchie, his elbow is ouchie, his shoulder is ouchie. Something else is going on.”
I look at the whole dog. I come up with a plan and I write all the list for the owner. I’m like, “These are the things I see and these are my goals for your dog.” Almost everybody, it’s – we are going to address pain because everybody has pain. We might be working on your flexibility. We might be working on your strength. Everybody needs core. All of us need core especially Tripawds. They need core work all the time.
Dr. Esquivel

When I come up with a plan, I sit down with the owner and I just have a general discussion with them about like this is what I saw, this is what I plan to do, these are the therapies that I recommend. Kind of set out a treatment plan for them.
And I’m going to give you homework. And in your homework are these exercises and you got to do them every day. Every day especially starting out.
I try to put some of the responsibility on the owner too. They have to be a participant in their care. They have to be an advocate for their dog. So I need them to be my partner and I need you to do your homework.
When you show up every week, you can’t lie to me and tell me that, “Oh yeah, I did it every day,” when I know your dog isn’t doing it because I can see it because your dog is not getting better. You can’t lie. Your dog tells me.
Dr. Esquivel
TRIPAWDS: it’s an equal partnership. I mean the pet parent is just as involved as the dog and you.
Dr. Esquivel: Yeah. And then you have to come up with ways because some dogs are treat-motivated. Sometimes they are owner-motivated. And so sometimes we have to have the owner there to get the dog to walk in the treadmill.
Sometimes we have to have – the owner has to lead them across on obstacles or something like that because the dog is just like, “Screw you! I’m not doing this. I’m just going to sit here.” So it kind of depends.
We really like the food-motivated dogs because they are easy to work with. But we got some dogs that do really great with their owners and we have other dogs that are like, “Yeah, can you wait in the lobby because your dog is trying to eat me because he wants to protect you.”
You’ve got to figure it out. I mean I have some truly aggressive dogs that come into my practice that they come in with a basket muzzle and we just try to figure out what their triggers are. And even if the dog is aggressive, there are works around and there are fear-free ways to do things with them too. And you just got to know what their trigger is. You got to work around it.
Dr. Esquivel
The point is, I come up with a plan and I set it out for them.
I have a discussion with them and basically, it’s asking for the owner to commit to initially like a Tripawd – we do usually do like a week-long or a week – an appointment a week is what I’m trying to get at.
We will say come in once a week. And we do that for 6 to 8 weeks, 8 to 12 weeks. It kind of just depends on what I see. And that’s kind of my general recommendation for pretty much anybody because I want them to get used to coming.
I want them to understand that we are not the regular vet.
If there dog is really nervous, it might take us 2 or 3 tries before they even get in the treadmill, before we even turn on the water, before they even start walking.
We try to do it as positive reinforcement. And so, getting the dog used to all these new things and getting them to be comfortable coming into our practice so that when they come see us, they are excited to come see us and it’s not scary.
We get that commitment from them like, “Hey, we want you to come every week for 2 months.” And then after that, I do a reevaluation. I take a look and I basically do a kind of an abbreviated version of my initial exam. So it’s a little shorter exam and basically just rechecking the things that I’m like, “Oh, that leg was a little less flexible,” or I want to see that the muscles are improved on this side or if they’ve got atrophy on one side, I want to see that they are actually evening out on both sides. And how are they standing? Are they walking better? Are they lame still? Or do I not see the lameness at all?
After that follow-up, then I adjust. And most of my patients, unless they are really young dogs, we might see them periodically if they have – basically we say once we graduate from therapy, “Come see us when you need us again.”
Dr. Esquivel
When they have a new injury or flare-up of whatever the injury is. I try to give the option to if possible, to go to more of a maintenance.
I think of these dogs especially the older dogs as a long-term project. That we need to get these dogs to a maintenance.
And every dog is different. So some dogs especially at end of life, it’s more like we might get to every other week or even monthly and then we kind of go back to every week once the winter hits or something and they’re having a flare-up.
My kind of middle-aged dogs to younger dogs, they might be coming twice a month. They might be coming once a month. They might only come see us if they think like, “Hey, he is not moving as well,” and we might deal with that flare-up for a couple of weeks, get them back to where they were, and then we let them go again. So it kind of varies on the pet and what’s still in line. But these guys, especially Tripawds, they are a forever client.

TRIPAWDS: I presume the goal is to help get the animal to the point where it doesn’t need such intensive therapies regularly?
Dr. Esquivel: Correct.
TRIPAWDS: If somebody doesn’t have access to a really awesome therapy center like yours, what are their options?
Dr. Esquivel: Right. So I live in New Mexico. It’s very rural and definitely therapists are few and far between. Like you say, we’ve got – there’s a practice in Santa Fe, there is my practice in Albuquerque, and there’s a practices in Las Cruces and that’s pretty much it for the whole state.
I will occasionally get clients that will drive 2 hours to come see me from Arizona, from the southern half of the state. I’ve had I think somebody come from like El Paso. Nobody is near them. So they turn it into a day trip kind of thing.
What I try to do for those people is give them a plan. This is the plan I want you to stick to whether I can see your dog or not. And obviously, there are some things that you can do at home and there are things that I can do here. Everybody doesn’t have an underwater treadmill in their home. So how can you modify things to just – at least do the basics and a lot of that is more the exercises than anything and just being able to recognize like, “Hey, when do you really need to go see your vet and when is it a problem for your particular case?”
Dr. Esquivel

I do have people that travel to see me even just for the one time and I try to basically set them on a path.
There are resources out there. Obviously, you guys do a great job of advocating for Tripawds and you guys provide some of that, there are YouTube videos, there are online Facebook groups that dogs living with disabilities kind of thing. There are a lot of different resources out there that you can find for examples of how to do a specific thing. But it’s kind of general information.
Depending on where you live, in New Mexico, we are not allowed to do telemedicine, but there are some states where you’re allowed to do that. So you could go and see a therapist and establish a relationship with them.
And if you are in a remote area, you could hopefully do something telemedicine. And we are seeing that more and more in vet medicine anyway, but it really is state-dependent, like we are not allowed to do any kind of telemedicine type of things in the state of New Mexico.

TRIPAWDS: Even if it’s just that one evaluation and a lesson plan and then some periodic follow-ups, what would someone look for in a clinic, a rehab-specific clinic aside from the credentials. How do you choose if you do have – if you are lucky enough to have choices?
Dr. Esquivel: Finding a certified therapist would be ideal. If you can find somebody and there’s little search engines on those programs that say, “Find a therapist and put your state in.” And hopefully you can find somebody who is certified.
I do know there are some general practitioners out there that have gone to CE meetings and things like that and they do have lectures that are very general and they are just, “Here’s how to start a rehab program in your practice.”
There are some general rehab or I should say some general veterinarians that do have a little bit of rehab knowledge and can touch on it but I would hope that your general practitioner who has no idea would say, “Hey, I don’t know or let me find you somebody you could to talk to,” or they can use their network and say, “Hey, I have a colleague who actually does that in Colorado.” We get a lot of those on like our list that was like, “Hey, my client is moving to somewhere. Anybody doing a practice in that area?”
I would hope that your general veterinarian would be like, “I don’t know but let me find out. Let me find you somebody who can help you or point you in the right direction.“
TRIPAWDS: Thank you so much, Dr. Esquivel. It has been great fun and we hope to have you on again soon.
Dr. Esquivel: All right. Sounds good. Thank you.
[End of transcript]
 Join the forum discussion on this topic!
Join the forum discussion on this topic!